cRITICAL LANGUAGE
Critical language refers to the use of standardised communication in which specific terms or phrases have a clearly defined, mutually understood meaning.
Neck Rescue is the term used by the Vortex Approach to describe emergency cannula or scalpel cricothyroidotomy/tracheotomy procedures required during can't intubate, can't oxygenate (CICO) events. Unlike many other terms applied to this procedure (emergency surgical airway, emergency front-of-neck access, invasive airway access, infraglottic rescue, etc). Neck Rescue satisfies the criteria required of such a term in being simple, intuitive, precise, unintimidating and inclusive of both cannula/scalpel techiques performed on either the cricothyroid membrane or trachea.
Click at left to access link to an editorial on the importance of critical language in airway managment, published in the British Journal of Anaesthesia
TRIGGER
According to the Vortex Approach the trigger for initiating Neck Rescue is the inability to confirm alveolar oxygen delivery following completed best efforts at all three upper airway lifelines.
Note that this trigger is independent of the oxygen saturations since, even in the unusual situation where following best efforts at all three lifelines the oxygen saturations remain high, the inability to confirm alveolar oxygen delivery following best efforts at all three lifelines means that eventual desaturation is inevitable. Rather then being a deterrent to its performance, recognition of the need for Neck Rescue while the oxygen saturations remain high should be viewed as advantageous - providing increased time to perform this confronting procedure in a more controlled manner, thereby increasing the chance of success.
Conversely a critically low oxygen saturation is not in itself a trigger to initiate Neck Rescue if best efforts at all three lifelines have not been completed. While legitimate opportunities to enter the Green Zone in a timely fashion via the familiar upper airway lifelines remain, these should be exploited as they are more likely to be successful than resorting to an unfamiliar and more traumatic technique.
Thus oxygen saturations are not a relevant consideration in deciding the trigger for Neck Rescue - they are, however, a relevant consideration for determining how many attempts are reasonable before declaring a best effort at a lifeline in a particular situation. When the oxygen saturations are critically low it might be reasonable to have only one attempt at each lifeline before proceeding to Neck Rescue.
The accompanying video (left) addresses a number of concerns raised with the Vortex Approach including a detailed discussion of the rationale for performing Neck Rescue if the oxygen saturations are still high (note that this video refers to an older version of the Vortex that uses a slightly different graphich and nomenclature to the current version).
technique
Techniques for Neck Rescue are distinct from non-emergency techniques to access the airway via the anterior neck (e.g. surgical tracheostomy, percutaneous tracheostomy), which are inappropriate for the time critical situation of a CICO event. Both cannula and scalpel techniques for Neck Rescue have been described and there is no clear evidence for the universal superiority of one of these in terms of efficacy or safety. As such, the Vortex Approach does not advocate a particular CICO Rescue technique if best efforts at all three lifelines are unsuccessful. More important than whether a cannula or scalpel technique is used is that the clinician has decided, in advance, on the technique for CICO Rescue that they would initially use, having considered the following elements:
Cognisance: the clinician must be well informed of the efficacy and complications of different techniques for the management of CICO as they apply to their clinical practice and know in advance which technique is most appropriate in a given clinical situation. There should not be scope for indecision about the technique to be implemented once a CICO event arises.
Competence: the clinician and their team must be adequately trained in their chosen technique(s) (technical preparedness to perform Neck Rescue). Given the infrequent nature of CICO events, the competence of clinical teams in Neck Rescue cannot be achieved by one off training sessions but requires conscientious, repeated training at regular intervals to prevent skill attrition.
Capability: the clinical team must have immediate access to the resources required to perform their chosen technique. It is recommended that pre-packaged Neck Rescue kits are immediately available to facilitate access to the equipment required for whatever technique is preferred. The efficient implementation of Neck Rescue when it is needed also requires clinical teams to be trained in the process of priming for Neck Rescue using this equipment. In clinical practice priming for Neck Rescue has the ancillary benefit of providing additional opportunities to reinforce the process of escalating towards Neck Rescue even in circumstances where a CICO event does not occur. By encouraging familiarity with escalation towards Neck Rescue during more common difficult airway events, priming has the potential to overcome the 'taboo' of confronting the potential for Neck Rescue in everyday practice, thereby facilitating both the technical and psychological preparedness of clinical teams to deal with a CICO event when it does occur.
Context: the clinical team must have a clear understanding of when to initiate Neck Rescue. This requires that they are able to clearly define the clinical criteria that indicate a CICO situation exists (recognition) and can clearly and unambiguously communicate this to the rest of the team using consistently understood, standardised critical language (declaration).
Confidence: the clinical team must have the resolve to act when this potentially confronting procedure is required (psychological preparedness to perform the Neck Rescue).
Thanks to George Kovacs for his contribution to describing the 'foundation elements' of effective Neck Rescue
The above principles are consistent with the position of the Australian & New Zealand College of Anaesthetists in relation to Neck Rescue.
Videos demonstrating both the cannula and scalpel techniques for Neck Rescue developed at Royal Perth Hospital, as well as the technique for safe oxygen insufflation when using a cannula technique, are available via Dr Andrew Heard's YouTube channel.
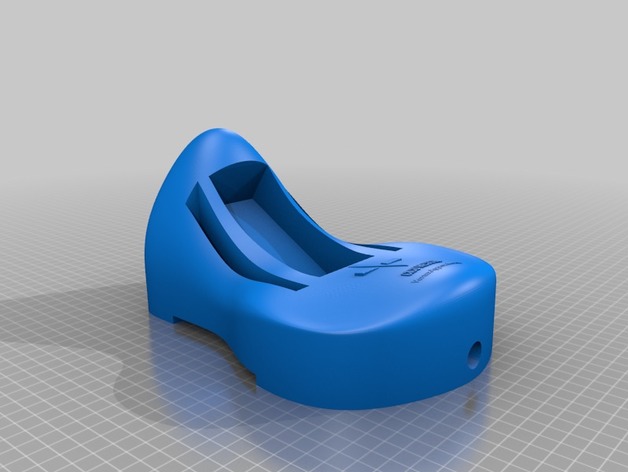
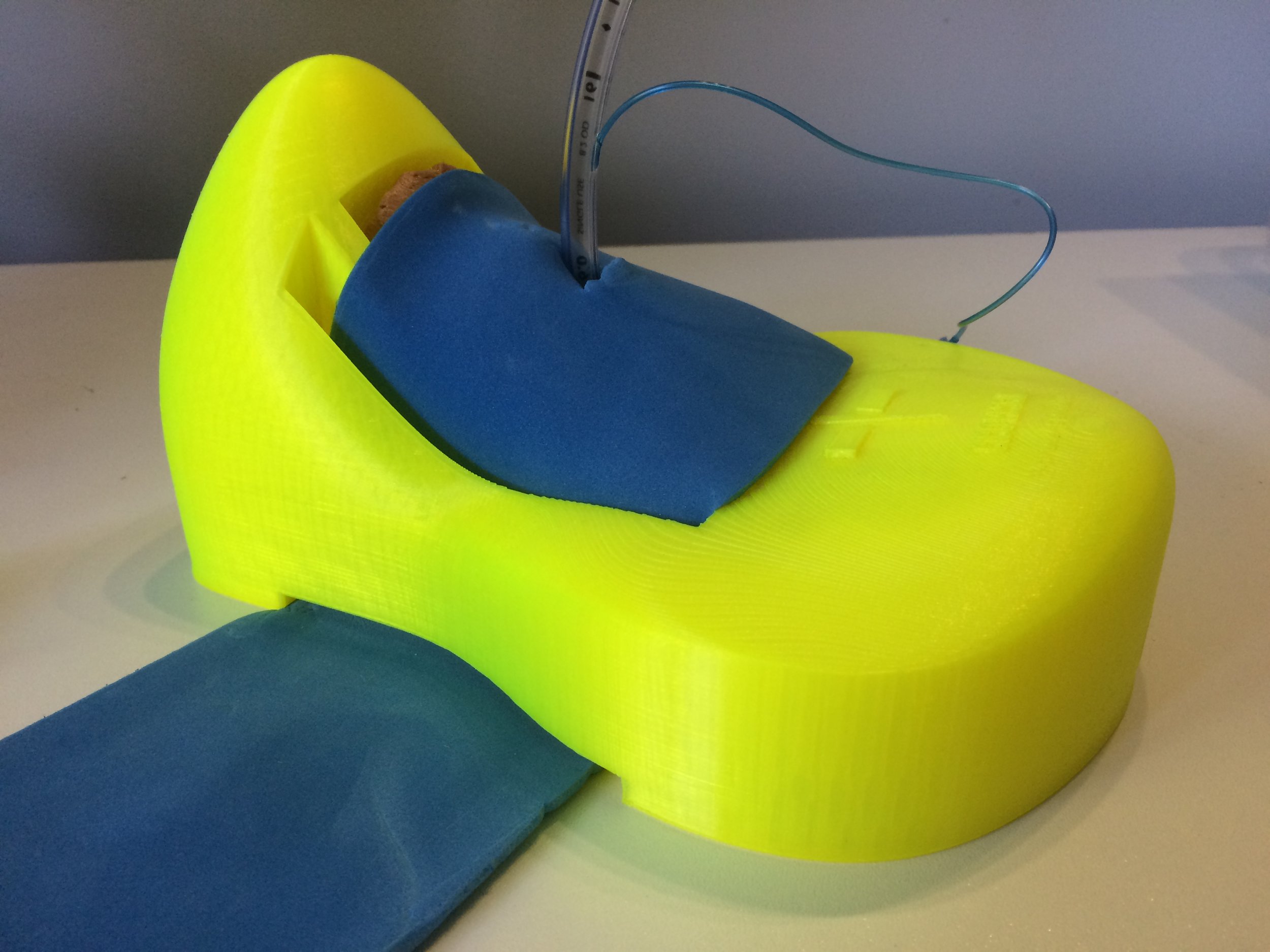
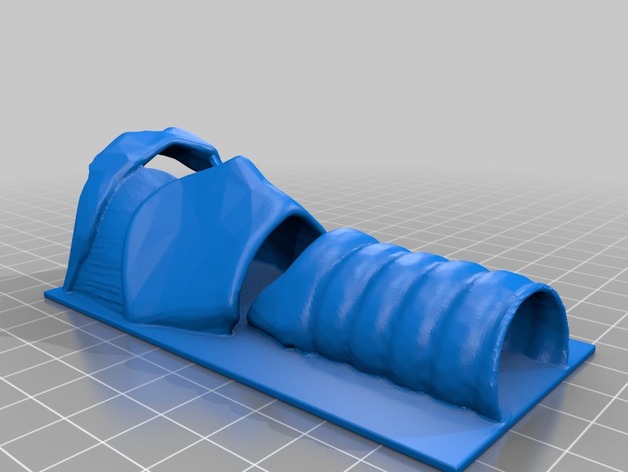
VORTEX 3D PRINTABLE Neck RESCUE TRAINER
The Vortex Neck Rescue trainer consists of 2 components: a larynx component that inserts into a neck baseplate to provide realistic anatomical features for practising of Neck Rescue techniques.
The laryngeal component of the trainer is based on original files by University of Dundee, BodyParts 3D and The Database Center for Life Science which have been extensively developed by Dr Andy Buck who also created the neck baseplate.
The infrequent and varied nature of CICO events makes obtaining clinical evidence of the best technique for Neck Rescue challenging. Developed by Dr Laura Duggan and the International Airway Collaboration, the Airway App provides a simple, anonymous method for clinicians to share their experiences of Neck Rescue (& awake intubation) and so increase the knowledge base in this area.
Click on the image to the left to download the app.